COVID-19
 Monitoring Ventilation to Reduce the Risk of COVID -19 Transmission
Monitoring Ventilation to Reduce the Risk of COVID -19 Transmission
As part of our community science activities, we have designed a second-generation device capable of long-term monitoring of indoor air. It is used to assess and improve ventilation, an extremely important factor in COVID-19 transmission, especially during the winter months.
Our work on this began last year when we sponsored a workshop at Dublin High School called Expedition CO2, aimed to increase awareness of the sources and sinks of carbon dioxide, an important greenhouse gas, in our environment. Middle and early high school girls designed and built first-generation CO2 sensors to study photosynthesis, human and animal respiration, combustion and fermentation.
Why Measuring CO2 is Important
The more we make indoors look like outdoors, the better we can eliminate or significantly reduce COVID transmission. Opening windows and doors even slightly to the outside are simple ways to increase ventilation and lower risk. The concentration of carbon dioxide (CO2) indoors is a measure of how much of the air we are breathing comes from other individuals in the same area. Around 4-5% of each outgoing breath contains waste CO2 from our bloodstream (the average adult human breathes out 1kg of CO2 per day). Because of this, the indoor CO2 concentration is proportional to the amount of air expelled by other people and quality of room ventilation. If all people inside a building or room are healthy there is no risk of airborne virus transmission but if one or more are asymptomatic then others will be exposed.
Engaging students in our Monitoring Program
Our new Quest high school intern, Ethan Hui, is working with us to design a custom electronic printed circuit board for the CO2 monitor. Ethan comes to Quest through a collaboration with ‘lolani School in Hawaii. With a printed circuit board for assembly, it will be relatively easy for anyone (from middle school on up) with basic soldering skills and some online mentoring to build a sensor for themselves.
During January we have been testing a small number of CO2 monitors in homes and a few public spaces. So far, Quest has baseline data from a local library, a number of homes, and a private, in-person elementary school. These “smart” sensors can store and plot data on a publicly available website and clearly show the effects of opening windows and doors to dramatically improve ventilation and lower COVID transmission risk.
At the end of February we will start loaning a limited number of monitors to interested students and families for up to 2 weeks so that they can explore ways to improve indoor air quality. We are also seeking both public institutions and private businesses who are interested in using the monitors to assess their work spaces and mitigate indoor risks.
If you are interested in more information contact Rick Stulen (rstulen@quest-science.org) or Caleb Cheung (ccheung@quest-science.org).

Hello! My name is Ethan Hui, and I’m a high school senior at ‘Iolani School in Honolulu, Hawaii. I am interested in designing, prototyping, and working with electronics and robotics.
I am currently working with Quest Science Center director Dr. Rick Stulen to design a custom printed circuit board for a carbon dioxide sensor.
I am excited to work with Dr. Stulen on this carbon dioxide sensor because I hope to get some experience designing printed circuit boards and get to know about the real-life process used towards creating presentable products.
 COVID-19 Vaccines: What you Need to Know About Rapid Development, Safety and What it will Take to Stop the Virus.
COVID-19 Vaccines: What you Need to Know About Rapid Development, Safety and What it will Take to Stop the Virus.
By Alan Burnham
The COVID-19 virus has only been circulating for about a year, but vaccines are being approved at a rate unprecedented in the history of medicine. In this article, I look at how we’ve been able move so fast and why it’s so important to get vaccinated despite the politicization of the disease and the numbers of people who mistrust vaccines.
How have the COVID-19 Vaccines Been Developed So Fast?
Two factors provided the scientific foundation for rapid vaccine development: the discovery and research around DNA, and cancer research. First, we need to step back to 1953 and the discovery of the double-helix structure of DNA, deoxyribonucleic acid. This discovery is the foundation of molecular biology, which includes a chemical understanding of the genetic code of living organisms. Of course, life is more complex than just DNA, including the existence of life forms that use ribonucleic acid (RNA) for their genetic code and the debate over whether or not viruses are a life form even though they have a genetic code based on either RNA or DNA. I’ll pass on that debate for now.
The next step in our story is the “war on cancer” started by President Nixon in 1971. It was also called a “moonshot”, reminiscent of the Apollo program of the previous decade. Although many have said that the war failed, because it did not cure cancer in short order, others state unequivocally that its ultimate impact has been extraordinary. We are not there yet, but progress is significant. But as is often the case for basic research, it has yielded unexpected side benefits, e.g., it laid the foundation for this year’s phenomenal progress on a COVID vaccine.
How did the COVID-19 vaccines get developed so fast?
- Years of experience developing similar vaccines
- Advances in technology, like DNA and RNA analysis
- Massive infrastructure that has been deployed to support trials and evaluate data
Types of COVID-19 Vaccines
All COVID-19 vaccines are based on knowledge related to our understanding of the molecular biology of the SARS-CoV-2 virus. The various vaccines differ in detail how they use this information to enable our body to recognize and attack the invaders. Some new vaccines use the genetic code to directly stimulate your body to create antibodies, a direct result of our ability to both sequence and manufacture genetic material rapidly. Other “old school” vaccines use parts of or weakened virus cells to trigger an immune response.
DNA and RNA analysis is fast, relatively inexpensive, and used in many scientific disciplines. Ancestry and 23andMe sell rudimentary DNA analysis for people for about $100. A Chinese lab sequenced the RNA genetic code of the SARS-CoV-2 virus within weeks after it was discovered and before most Americans had even heard of it. The virus mutates slowly, and tracking those RNA mutations can help trace the migration pathways.
It wasn’t always that way. While in grad school, I was a teaching assistant for a biophysics class taught by Olke Uhlenbeck, whom some call the father of RNA. Genetic sequencing was relatively new then (nearly 50 years ago), and I remember him saying once in class that he doubted the human genome would be sequenced in our lifetime. But then came microprocessors for automating lab equipment, supercomputers for linking short segment sequences into a full sequence, and the Human Genome Project, which included Lawrence Livermore National Laboratory’s participation as part of the Joint Genome Institute.
Returning to the initial question, how did the vaccines get developed so fast? It is really a combination of traditional experience, huge advances in technology, and a real sense of urgency. Human trials still take weeks to months, but the supporting infrastructure can now facilitate those trials and analyze the data much faster. Such clinical trials cannot evaluate the likelihood of delayed side effects, but neither can our current understanding of COVID quantify the long-term health effects of that disease.
How important is it to get vaccinated? Here’s a look at the numbers.
- COVID-19 has a basic reproduction number (R0) of 3.
This is how many cases on average will occur as the result of a single person who is affected. An R0 of 3 means the virus will spread exponentially. - The only way to stop COVID-19 from spreading enough so that it dies out is to reduce the effective reproduction number (Rt) to less than 1.
- Masks and social distancing have reduced the Rt to between 0.8 and 1.5, enough to slow, but not stop the virus.
- The Solution: We must immunize most people – 78% – unless we want to keep wearing masks and staying home indefinitely.
Are the COVID-19 Vaccines Safe? Are they Necessary? The Answers Lie in the Numbers.
All human activities involve some risk, and a large part of life is balancing risks, both for ourselves and the people we come in contact with. We don’t yet fully know the precise risks of the COVID vaccines, but they are certainly less than those of the disease. Undiagnosed low-to-no symptom cases cause uncertainties, but using antibody tests to estimate undiagnosed cases, true hospitalization and death rates are about 4.5% and 0.4% respectively. Those are 10,000 or more times greater than for typical vaccines. There are reports of allergic reactions to the Pfizer vaccine, but they are short-lived—a day or less. Nevertheless, those who have a history of allergic reactions are advised to wait.
That brings us to the final question of this topic, how many people need to be vaccinated to prevent another pandemic? We’ve all heard about herd immunity. That occurs when the chance of someone infecting someone else becomes less than one, which leads to exponential decline rather than exponential growth.
By now, most of us have heard of the reproduction number, even though some might be confused between the basic reproduction number (Ro) and the effective reproduction number (Rt or Re). The former is the number of people a person infects in the absence of any measures. Ro for COVID is about three. That is only half as infectious as pertussis, rubella, and polio and only about a quarter as infectious as measles, chickenpox, and mumps.
Up to now, we have used masks and social distancing to reduce the spread of COVID. The effective reproduction number has varied between 0.8 and 1.5 as people change their behavior. The fraction of the population that has gained immunity from catching and recovering from the disease is still less than needed for herd immunity, but perhaps as much as 30% of the population after considering no-to-low symptom cases. For the effective reproduction number to become less than one without masks and social distancing, about 70% of the population would have to become immune by recovering from the disease or being immunized, i.e., Re=(1-0.7)*3=0.9. If a vaccine is only 90% effective, then about 78% of the population must get shots or have recovered from COVID to achieve 70% immunity.
The calculation gets more complex when one includes how many people have already attained immunity through having COVID, whether we know who has achieved that immunity, how long immunity lasts, and statistical uncertainties and distributions. However, the simple conclusion is that the shots must be highly effective and most people need to get the shots—the important number is three times the product of those two factors. So it is clear from a public health perspective that public willingness to get immunized is just as important as the effectiveness of the vaccine. Although the basis for his prediction has not been described in detail, Dr. Fauci now predicts that herd immunity can be attained by late spring or early summer, presumably from the combination of those vaccinated and those becoming immune by the virus, including the large number of asymptomatic cases.
 Demystifying How Masks Work
Demystifying How Masks Work
By Alan Burnham
Masks are a major tool against the spread of COVID other respiratory problems such as those related to smoky air, but separating the science from folklore can be tricky. In this article, we explain how masks work, how effective they are against various threats, and how to make and use masks most effectively.
Masks use a variety of means to filter out different kinds of particles and chemicals such as straining, impaction, diffusion, electrostatic attraction, and absorption. Their relative importance depends on the situation, and understanding the difference is key to understanding what N95 means.
Masks for Straining and Absorption
Using a mask for straining (like when you cook pasta) is effective only during the worst dust storms or when someone is coughing or sneezing directly in your face because most particles are too small to be strained. Masks for absorption are important only when you work in an environment with lots of solvents or to protect yourself from chemical warfare agents.
Masks for Impaction and Diffusion
Impaction filters particles greater than about 1 micron (a human hair is about 200 microns). The particles can’t follow the gas streams passing through the mask because they can’t turn fast enough, so they run into a fiber and stick. Diffusion comes into play with particles that are less than about 0.1 micron. These particles move around a lot (diffuse) when they are going through the mask, so they are likely to strike a fiber and stick. It is those pesky particles between 0.1 and 1 microns that are the most difficult to filter—the size of a COVID-19 virus.
Masks for Electrostatic Filtration: N95
N95 masks are most effective because they have polarized fibers that can attract charged particles of all sizes. That helps fill in the valley of bad filtering efficiency. You can take a sidebar to this excellent video that explains these mechanisms in more detail.
So, What Does N95 Mean, Anyway?
N = Not effective for filtering oil mist. (R rated masks do work on oil mist.)
95 = Filters out 95% of the particles
Most popular descriptions don’t explain that N95 masks filter 95% of those pesky particles between 0.1 and 1 micron, specifically particles with a diameter of 0.3 microns according to OSHA. A COVID-19 virus is only about 0.1 microns, but is usually coated by mucus, making them larger than 0.3 microns. This makes N95 masks the most effective for filtering the COVID-19 virus.
For comparison purposes, aerosol particles are typically defined as less than 10 microns. The Purple Air map so many of us used during the smoky air times uses a default value of 2.5 microns, much larger than the virus particles – which means the mask you used during the wildfires isn’t going to do the job when it comes to COVID-19.
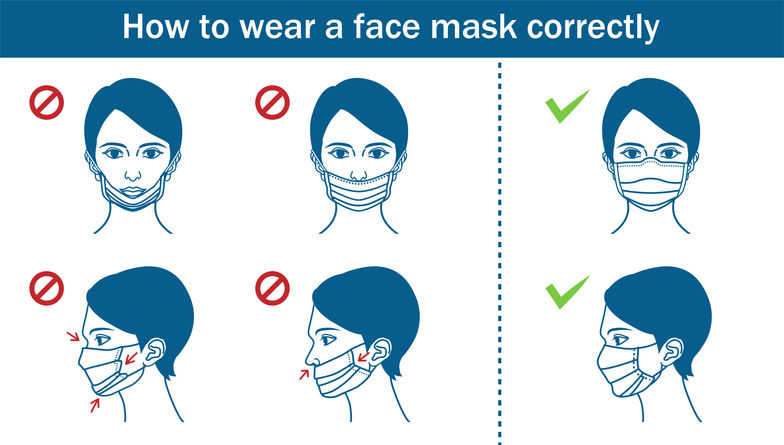
How and Why to Wear a Mask
To reach high efficiency, the mask must fit tightly to the face. If it doesn’t, the airflow will simply go around the mask rather than through it. Large exhaled droplets will go straight into the mask by impaction, but the smaller particles will follow the air streamlines and leak out the edges. The amount of leakage can be detected by using how temperature differences can bend light. This method is used and explained in this video.
Multiple layers of protection are better than one. If, for example, you are in a closed space where 80% of the viral emissions from sick people are captured in their mask and 70% of the escaped viral particles are captured by your mask, your risk of infection drops to 6% (0.2*0.3=0.06) of the risk from no one wearing a mask. The exact risk reduction depends on lots of factors, but the math is clear—two layers of imperfect protection is always better than one layer of imperfect protection.
A lot has been made about the motivation for wearing a mask. The primary justification is and should be that it prevents you from making others sick. More than half of COVID-19 transmissions occur from people who have not yet developed noticeable symptoms or are asymptomatic. In addition, capturing particles at their source is always more effective. But masks protect the wearer, also, which the CDC recently acknowledged, and two studies showed a 70% reduction in infections for those who wore masks.
 COVID-19: Know the risks and make good decisions
COVID-19: Know the risks and make good decisions
By Lee Younker and Gina Bonanno, October 21, 2020
COVID-19 risks and decision-making
Over the past eight months individuals and families have had to make decisions related to how they should behave during the COVID-19 pandemic. The decisions have covered all aspects of life including getting haircuts, visiting salons, dining out, gathering with friends and family, dentist and doctor appointments, shopping, using public transit, getting on an airplane, arranging for home repairs, house cleaning, and so on. These decisions are all related to how much risk is involved if we do these things, and what steps we can take to keep ourselves safe and to avoid putting others at risk. While county and state guidelines have sometimes helped, they have also at times been contradictory and confusing. The specific decisions we make on a daily basis have been difficult, and complicated by many uncertainties. Guidance from county and state health officials has sometimes been confusing and contradictory as experts have learned more about the virus and how it is transmitted.
In this edition of Quest’s feature Science in the News we look ahead at the projections of the pandemic over the next six months and have assembled a set of articles and studies that can provide context, background and an underlying framework to help inform decision-making in the time of COVID-19.
The Pandemic in the Fall and Winter: What to expect and prepare for
Since March, over eight million Americans have tested positive and over 221,000 people have died1. Many experts believe these numbers are undercounted due to inadequate testing and the cause of death not always being appropriately assigned to COVID-19. Clearly, the recent acceleration in the rise of cases in the US and worldwide indicates that we are certainly not near the end, and many in the public health arena believe we are entering a very critical and challenging period. Although it varies widely across the US, cases are rising in the majority of states and a number of states are setting ominous seven-day records for infections and hospitalizations. Several recent studies have concluded that 85 to 90% of Americans are still vulnerable to the virus. The virus is out there in large quantities and most of the population is still under threat of infection.
Adding to the concerns posed by the numbers, there are several aspects of the fall and winter seasons that are likely to exacerbate the unease. These include the colder weather driving more people inside where the threat of spread is greater, a seasonal flu and COVID-19 double whammy potentially overwhelming medical facilities, outbreaks occurring in schools and colleges and spreading to the broader community, fall and winter holidays encouraging large gatherings, and the distinct possibility that pandemic fatigue could cause people to lower their guard. Given the current alarming numbers and the fall and winter factors, some models suggest over 360,000 deaths by the end of the year.
Understanding the risks
The key to making good decisions about activities and behaviors is to fully understand all the elements that underlie COVID-19 risk. Because the virus is new and the situation has been dynamic and evolving, it has been difficult to get full agreement on the best way to think about and characterize the risk. There is an emerging view on the three key elements defining risk in any setting: prevalence in the community, exposure and individual factors.
- Prevalence: The first element defining risk is the extent to which the virus is present and circulating in a community or county. A group led by the Harvard Global Health Institute has provided an interactive map and dashboard showing COVID-19 risk in counties across the country. The approach is based upon the number of new daily cases per 100,000 people. They use this metric to show the severity of your county’s outbreak.
- Exposure: Once you know the level of virus spread in your community you need to understand how the virus is actually transmitted from person to person. There has been much discussion and debate on transmission over the past months with respect to contaminated surfaces, droplets and aerosols with most experts concluding that aerosols are the most effective transmission mechanism. Erin Bromage, an Associate Professor of Biology at the University of Massachusetts Dartmouth has synthesized the information and provided a very concise and easily understood summary of where and how the virus can get passed from person to person. Hint: it is not opening the mail or passing a jogger on the bike trail, it is close interactions in a poorly ventilated indoor setting for a significant period of time. If you understand the transmission mechanisms, you are better equipped to assess risk levels associated with various activities from opening the mail to going to a bar. The Texas Medical Association has developed a one-page guide defining how risky an activity is on a scale of 1 to 10. For anyone wanting more detailed information on the science of aerosol transmission of COVID-19, an extensive set of FAQs entitled, FAQs on Protecting Yourself from COVID-19 Aerosol Transmission , has been compiled based on the collective research of scientists and engineers from around the world.
- Individual factors: The final element that is essential to the overall risk assessment is related to the individual. There are very consistent trends in the data related to how individuals are impacted by the virus, including more deaths among men, deaths that skew heavily toward the elderly and minorities and higher death rates in individuals with underlying health problems. The Mayo Clinic in an article entitled COVID-19: Who’s at higher risk of serious symptoms? provides an excellent summary of this data. Medical conditions and demographics are not the only factors that play into an individual’s risk and decision-making. Behavioral scientists at the University of Pennsylvania , are finding that when presented with the same risk assessment data individuals can make very different decisions based on their personal biases, anxieties and stress responses.
Life must go on; balancing risks and benefits
According to Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, successfully developing and implementing a vaccination program that reaches the necessary number of Americans along with good public health practices, could result in something approaching normal by the end of 2021. At that point we would have endured nearly two years of disruption.
Clearly, we have to do more than understand and minimize risk. We need to find ways to safely do what we need to do and what we want to do. We need to find a way to balance risk and the benefits. Benefits in this case can be whether or not to proceed with an elective medical procedure or, for seniors, to visit children or grandchildren they haven’t seen since before the restrictions imposed by the pandemic. Assessing risk versus quality of life is something we’ve all been doing since the beginning of the pandemic, doing so based on data and science-based guidance can help minimize risk while allowing us to continue some aspects of our pre-pandemic lives. A new model by a group at University of Colorado and reported on by National Geographic provides an interactive tool that estimates the risk of aerosol-based transmission for a different activities based on the infection rate in your area and other parameters you can adjust to help understand what has the biggest effect on transmission risk. A group from MIT in a paper entitled “Rationing Social Contact During the COVID-19 Pandemic: Transmission Risk and Social Benefits of US Locations” addresses the question of what types of stores and activities should be open and what types should be shut down during surges of the pandemic by analyzing both the benefits and risk of the operations.
Looking to the future what are the main takeaway points?
1) Assess your situational risks: Who you are, where you live, and what you do all matter when you assess your level of risk or the level of risk to family members.
2) Follow the “Fauci Five” public health guidelines in all that you do: Wear masks, avoid crowds, keep a safe distance, do things outside as much as possible, and wash hands frequently. Most public health experts assert that wearing a mask is “…one of the most powerful weapons we have to slow and stop the spread of the virus…”2. It is quite amazing that these simple public health guidelines are the same tools we had at the time of the Great Influenza 100 years ago. Dr. Robert Redfield, Director of the Centers for Disease Control and Prevention, has asserted that if we followed these guidelines we could have the virus under control in 4-8 weeks2.
3) Beware of pandemic fatigue. Don’t get lax and don’t underestimate the threat of a fall surge. The holiday season will be difficult. The things we all like to do–large indoor gatherings often with family and friends that have traveled from afar pose real threats as spreader events. When you visit with friends and family over the holidays do it wisely.
4) Recognize that this will not last forever. The international scientific assault on this virus has been relentless and nothing short of phenomenal. Sure, mistakes have been made and conclusions altered but the progress in understanding this virus, how it gets transmitted, what impact it has, how it might be treated, and how vaccines can be developed has been remarkable. We have every reason to believe that this scientific knowledge and experience when coupled with basic public health practices can in fact lead us back to a more normal life in 2021 as predicted by Dr. Fauci.
At Quest we hope this article and associated links will be helpful as you and your family navigate the next challenging phase of the pandemic. Working together with our families, our friends, our co-workers and our communities we can have a positive impact on the outcome.

September
ReQuestEd: Interview with Dr. David Svec – Quest’s Gina Bonanno explores COVID-19 through the eyes of Dr. David Svec, Chief Medical Officer at Stanford Health Care – Valley Care in Pleasanton, a health care provider on the front lines of the pandemic here in the Tri-Valley. Listen to the Podcast. Read the Transcript.
May
ReQuestEd: Interview with Dr. David Rakestraw – Quest’s Caleb Cheung interviews Dr. David Rakestraw about his work responding to the COVID -19 pandemic at the Lawrence Livermore National Labs (LLNL) and his development of a high school physics course using cell phone sensors
Interview with FormFactor CEO Mike Slessor about his company’s response to COVID-19: DOWNLOAD PDF
The Coronavirus Pandemic: How is Alameda County Doing? – Tracking data for Alameda County and the surrounding area to provide our region with a local analysis of the progression of the pandemic, by Rick Stulen, Quest Director
April
Local Makers Helping Frontline COVID-19 Workers – Learn how Quest Advisory Board Member June Yu and her husband Brian McGinnis designed a DIY 3D printed face mask for health workers
Understanding the Math behind the COVID-19 Challenge – A deep dive into the mathematics behind the pandemic and analysis to make the data more meaningful, by Alan Burnham, Quest’s Founder and CFO
A Q&A with David Galas – Learn about the origins of the quick-turnaround test that is now in production for COVID-19